Working With Pain. The Impact On Mental Health.
Working with recurring or persistent pain is not just uncomfortable or inconvenient. It deeply affects our mental health and wellbeing, our capacity to work and our personal relationships. Distressingly, it can also end in suicide if those affected are not adequately supported.
Despite a strong link between pain and mental health, the extent to which work-related pain impacts individuals and businesses remains largely misunderstood and neglected. In these times of changing attitudes towards mental health in the workplace, business leaders need to be aware of the signs that pain is taking a toll on someone’s mental health and the avenues that are available to offer help and assistance.
Current Knowledge:
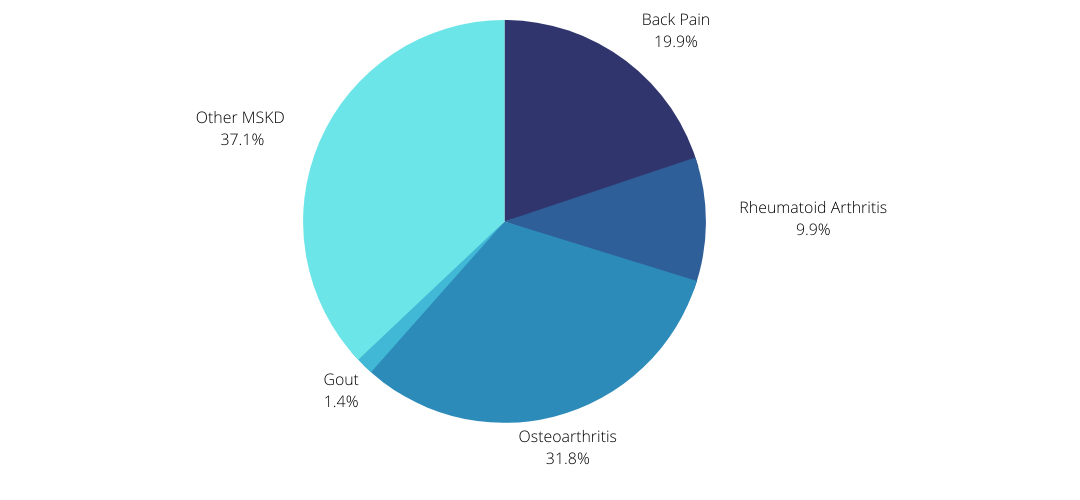
Australia spent more money on musculoskeletal pain-related conditions or injury than any other disease.
Australia Spent More Money (Over $12.5 Billion), On Musculoskeletal Pain-Related Conditions Or Injury Than Any Other Disease
Chronic pain costs Australia $73.2 billion dollars each year including $48.3 billion in lost productivity
One in five Australian adults with severe or very severe pain suffer depression or other mood disorders.
Major depression is the most common mental health condition associated with chronic pain, with among 30-40% of people with a diagnosed mental health condition also presenting for treatment for chronic pain.
Rates of mental health and suicide are higher amongst people living with pain.
High rates of generalised anxiety disorder, post-traumatic stress disorder and substance misuse are often present for people living with chronic pain.
Almost a third of Australian adults with severe or very severe pain experience high levels of psychological distress; around three times the rate of those with mild pain and six times the rate of those with no pain.
Suicidal behavior is also two to three times higher in people with chronic pain than the general population.
How To Tell If A Team Member Is Struggling With A Pain Condition
The complicated relationship between pain and mental health makes it difficult for employers to identify that a team member may be struggling with a pain condition. The signs may include:
Reduced productivity
Looking tired and stressed
Turning up late to work
Drinking more alcohol than usual
Taking extra leave
Taking illegal drugs
Constantly shifting position, stretching or rubbing a body part during meetings
Withdrawal from social activities
Increased irritability or moodiness
Having trouble concentrating, making decisions or multitasking
These signs can easily be misinterpreted and those living with a pain condition are often unfairly labelled as lazy and unreliable, antisocial, difficult to work with, irritable or uncooperative. Such misperceptions can lead to inappropriate responses from employers, such as disciplinary action or performance management, that only lead to further psychological distress and exacerbation of underlying mental health issues.
What To Do If You Suspect A Team Member Is Struggling With A Pain Condition?
Start the conversation and be prepared to listen
Many employers will be hesitant to take the initiative and offer assistance to a team member they suspect may be affected by pain due to concerns that they may be ‘opening a can of worms’ or inviting a Workcover claim. This attitude is counterintuitive and helps no one. Failing to take steps to identify the underlying reasons for an uncharacteristic change in a team member’s behaviour or performance and take appropriate steps to assist them will only prolong the situation and allow physical and mental health issues to become chronic and debilitating.
You don’t have to have all the answers and won’t be able to solve their problems but, as long as you choose the right time and place, listen non-judgementally and demonstrate kindness and empathy, they’ll be more likely to feel at ease and ask for help.
It helps to prepare yourself with some information about mental health support services and helplines that you can recommend, should the need arise. If you feel you’re not the right person to start the conversation. It may be someone from HR or your organisation’s Employee Assistance Program may be better suited to the task.
Respond To Your Team Member’s Needs
Whether or not an individual’s pain condition has resulted from performing their work tasks or is related to some aspect of their workspace, it’s crucial that these issues are identified and addressed without delay. You can do this by listening to their needs and providing or directing your team member to appropriate supports.
This might include:
Advising them to seek advice from their GP or other appropriate medical professional
Engaging a qualified occupational health professional to undertake an ergonomic assessment of their workspace to identify any issues with the worker’s tasks, workload, equipment or workspace design that may be causing or contributing to their pain.
Providing access to mental health first aid services or employee assistance programs and ensuring that your team are aware of these services and know how to access them.
Considering ways in which you can lighten their workload by delegating duties elsewhere or modifying their existing duties.
Follow Up Afterwards
It’s important to follow up on any conversation or actions taken. Check in with your team and ask them how they’re feeling and if they can manage their work better than before. Reassure them that you are still there to offer help if needed.
Don’t be disappointed if they haven’t acted on your advice to seek help. People will get support in their own time. Stay in touch and show you care. Even if you do not talk about the issue again, just knowing that you are there can make all the difference to a person in need.
Suicide Prevention
If your team member talks about harming themselves or suicide, it is important that you take them seriously. Do not get angry or upset. They will only feel guilty and it will make things worse. Instead, tell them that these thoughts are common but it does not mean that they have to act on these feelings.
Ask them if they have made any plans to end their life. If they have, stay close by and make sure they are not left alone.
If the person’s life is in immediate danger call triple zero (000) and remain with them until help arrives.
Access confidential mental health advice and support by calling mental health helplines such as Lifeline on 13 11 14 or Suicide Call Back Service on 1300 659 467
Where to get help
Your doctor
Lifeline, call 13 11 14
SANE Australia, call 1800 18 SANE (7623)
Beyondblue, call 1300 22 4636
Suicide Call Back Service, call 1300 659 467
We believe everybody has the right to feel safe and supported at work. Contact us to find out how we can work together to ensure the wellbeing of your staff is a priority. Contact Us